Key Takeaways
-
Medicare Part C, or Medicare Advantage, offers an all-in-one alternative to Original Medicare, but often comes with trade-offs in provider choice, coverage limitations, and out-of-pocket unpredictability.
-
In 2025, understanding plan structure, coverage networks, and coordination with Medicare Parts A, B, and D is critical before enrolling in Medicare Part C.
Understanding What Medicare Part C Offers
Medicare Part C, also known as Medicare Advantage, is a private plan alternative to Original Medicare. When you enroll in a Part C plan, you receive your Medicare Part A (hospital) and Part B (medical) benefits through a private insurance company that contracts with Medicare.
These plans are required to cover at least the same benefits as Original Medicare, but many offer additional features such as dental, vision, hearing, and prescription drug coverage. The appeal is strong: one card, fewer providers to coordinate with, and extra perks. But simplicity doesn’t always equal the best value or flexibility.
The Trade-Off Between Convenience and Control
You might be attracted to Medicare Advantage because it seems to simplify everything. Instead of juggling Parts A, B, and D separately, you get it all bundled. However, the simplicity comes with restrictions you may not anticipate.
Here’s what you give up:
-
Choice of providers: Many Part C plans rely on Health Maintenance Organization (HMO) or Preferred Provider Organization (PPO) structures. These networks limit which doctors and hospitals you can use without paying extra. Out-of-network care is often restricted or expensive.
-
Geographic limitations: Your coverage may only apply in a certain area. If you travel or spend part of the year in another state, your access to care could be limited.
-
Referrals and approvals: Some plans require prior authorization or referrals to see specialists, adding extra steps to your care.
In contrast, Original Medicare allows you to see any provider nationwide who accepts Medicare, without referrals or network restrictions.
Out-of-Pocket Costs: What Looks Predictable May Not Be
One reason many people lean toward Part C is the perception of cost savings. While some plans may advertise lower monthly premiums compared to Part B alone, that doesn’t tell the whole story. Here’s why:
-
Copayments for every service: Instead of paying a flat coinsurance rate, you might face separate copays for doctor visits, labs, imaging, hospital stays, and more.
-
Annual out-of-pocket maximums: In 2025, Medicare Advantage plans are required to cap your in-network out-of-pocket costs at $8,850. This limit helps protect you in high-use years, but it doesn’t account for out-of-network costs, which may have a separate and much higher cap.
-
Extra fees for additional benefits: While many plans include dental or vision, those perks may come with usage limits or copayments that you didn’t expect.
Original Medicare doesn’t have an out-of-pocket maximum, but most people add a Medigap policy for financial protection, which can be more predictable over time.
The Impact on Prescription Drug Coverage
Most Medicare Advantage plans include drug coverage, but the quality of that coverage varies widely.
-
Formularies are different: Each plan sets its own list of covered medications. If you take a specific drug, check that it’s covered and at a reasonable tier.
-
Pharmacy networks matter: Just like with provider networks, you may have to use certain pharmacies to avoid extra costs.
-
Annual changes: Plans can change their drug list and pricing every year. What worked for you this year might not be the same next year.
If you choose Original Medicare, you would typically enroll in a standalone Part D drug plan, giving you the ability to comparison shop without changing your medical coverage.
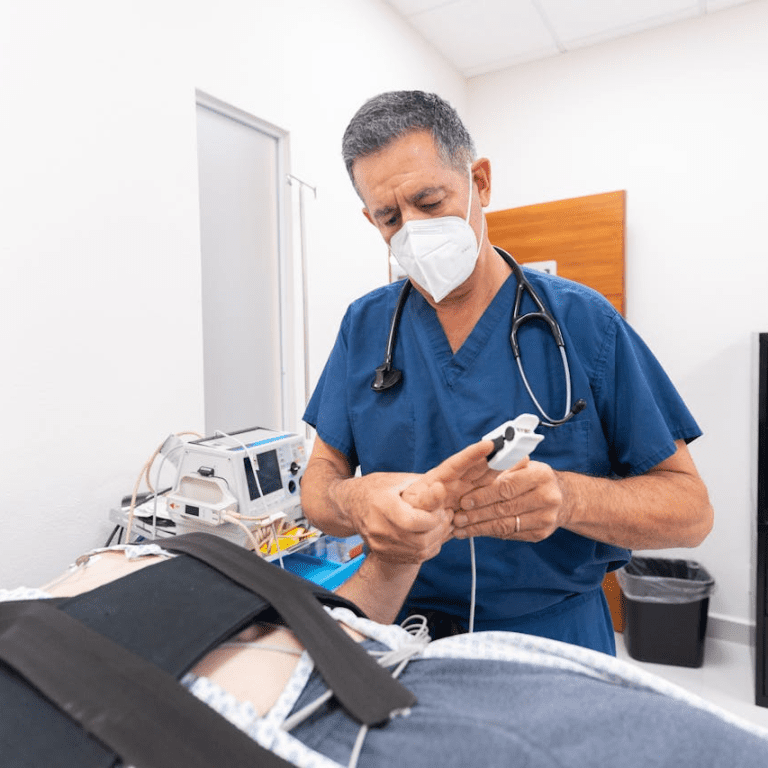
Care Coordination May Feel Streamlined, But Can Limit You
Medicare Advantage plans are designed to encourage care coordination. This can be a benefit if you have multiple conditions and need help managing care. Many plans offer nurse hotlines, care managers, or wellness incentives.
However, coordination can also mean oversight:
-
Utilization reviews: Your care might be delayed if your plan requires review before approving a test or procedure.
-
Formularies and treatment protocols: Plans may guide doctors to follow specific step therapies or formulary protocols that don’t match your needs.
With Original Medicare, your providers have more freedom to determine what care is medically necessary, without needing plan approval.
What Happens If You Want to Switch Later
This is one of the most overlooked aspects of choosing Medicare Advantage.
If you start with Medicare Advantage and later decide you want to move to Original Medicare with a Medigap policy, you might not be able to do so without restrictions. Here’s why:
-
Medigap underwriting applies: If you try to buy a Medigap plan after your initial enrollment period, the insurer can review your health history and deny you coverage or charge more.
-
Limited enrollment periods: You can only switch during the Annual Enrollment Period (October 15 to December 7) or Medicare Advantage Open Enrollment (January 1 to March 31).
-
Network disruptions: If your preferred doctors or hospitals leave your plan’s network, you might have to change providers mid-year unless you switch plans entirely.
Starting with Original Medicare and Medigap gives you the flexibility to switch drug plans annually without risking medical coverage changes.
Evaluating What Matters Most to You
Choosing between Medicare Advantage and Original Medicare isn’t just about costs. You need to consider your lifestyle, health needs, and preferences.
Ask yourself:
-
Do you travel often or spend time in multiple states each year?
-
Is it important to keep your current doctors?
-
Are you managing multiple health conditions that might require specialists?
-
Do you want predictable costs, even if premiums are slightly higher?
-
How much flexibility do you need in choosing providers?
The answers to these questions can steer you toward the plan that supports your health and financial goals in the long run.
Annual Reviews Are Non-Negotiable
Even if you pick Medicare Advantage and feel good about it in 2025, that decision isn’t permanent. These plans change every year. Your provider network, drug list, benefits, and out-of-pocket costs can shift from one year to the next.
That’s why it’s essential to:
-
Review your Annual Notice of Change (ANOC) every fall.
-
Compare your current plan to others during the Annual Enrollment Period.
-
Be proactive about switching if your plan no longer meets your needs.
Too many enrollees auto-renew each year without realizing what has changed. That inertia can be costly.
Why Simpler Isn’t Always Smarter
The appeal of simplicity is understandable. Medicare Advantage wraps everything into one plan, one card, and sometimes, one bill. But behind that ease can be hidden rules, restrictions, and unpredictable costs.
It’s not a one-size-fits-all solution. What seems easier today may create friction later if you lose access to a trusted doctor, face high out-of-pocket costs, or struggle to get services approved.
You owe it to yourself to look deeper before enrolling.
Make the Choice That Protects Your Future Health
Choosing a Medicare plan is one of the most important decisions you make for your health and finances. While Medicare Part C may appear to offer a convenient path, it comes with real considerations that can impact your long-term well-being.
Take time to review your options. If you’re unsure what direction fits your needs, speak with a licensed agent listed on this website for personal guidance.