Key Takeaways
-
Medicare costs in 2025 go beyond just premiums. You must factor in deductibles, coinsurance, out-of-pocket maximums, and potential penalties.
-
Understanding each part of Medicare and how it interacts with the others is key to making an informed, budget-conscious decision.
Medicare in 2025: A Breakdown of Costs You Can Expect
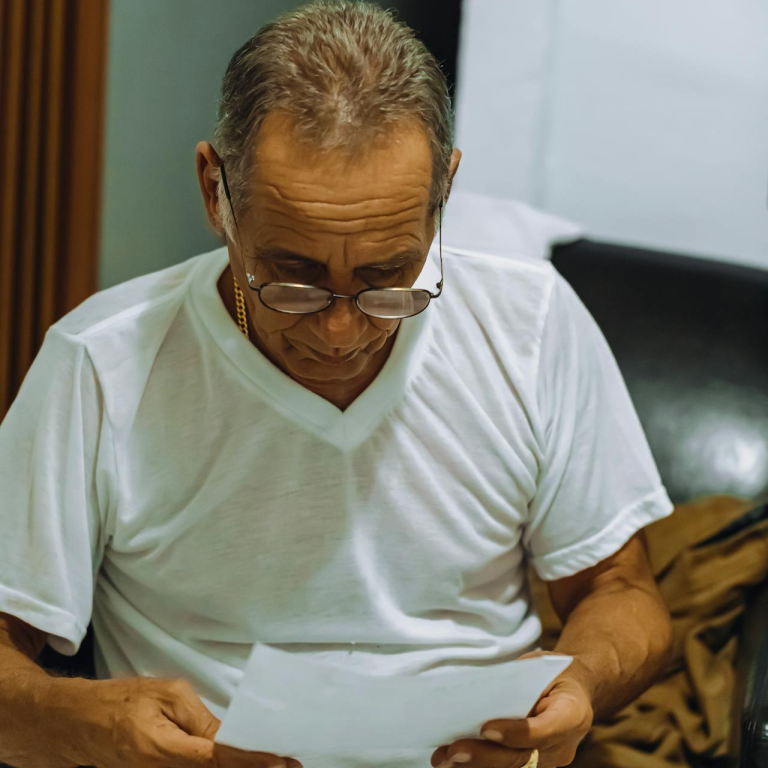
When you think about Medicare, your first thought might be the monthly premium. But the reality in 2025 is that Medicare involves a series of interconnected costs. Premiums are just one piece of the puzzle. If you plan on relying on Medicare for your healthcare needs, you’ll need to understand the full range of potential expenses—and what you can do to manage them.
Let’s look at what Medicare really costs you in 2025 and why preparing for these costs now can help you avoid financial surprises later.
What You Pay for Medicare Part A in 2025
Hospital insurance, also known as Medicare Part A, generally comes without a monthly charge if you or your spouse paid Medicare taxes for at least 10 years. But that doesn’t mean it’s free.
Here’s what you should know:
-
Premium: No monthly premium if you qualify based on work history. If you don’t, the premium is $284 or $518 per month, depending on how many quarters you worked.
-
Deductible: You pay $1,676 for each benefit period in 2025.
-
Coinsurance:
-
Days 1-60 in a hospital: No daily coinsurance (after the deductible)
-
Days 61-90: $419 per day
-
Days 91 and beyond (lifetime reserve days): $838 per day
-
Skilled nursing facility (days 21-100): $209.50 per day
-
These figures illustrate why it’s important not to assume you’re fully covered. A hospital stay, especially a long one, can trigger significant out-of-pocket expenses.
What You Pay for Medicare Part B in 2025
Part B covers outpatient care like doctor visits, durable medical equipment, and preventive services. This is where many enrollees begin to feel the financial pressure.
-
Premium: The standard monthly premium in 2025 is $185. Higher-income individuals may pay more based on income-related monthly adjustment amounts (IRMAA).
-
Deductible: $257 annually
-
Coinsurance: Once the deductible is met, you typically pay 20% of Medicare-approved amounts for most services.
You may also face excess charges if your provider doesn’t accept Medicare assignment. That’s something to keep in mind if you see specialists or receive outpatient care frequently.
What You Pay for Medicare Part D in 2025
Prescription drug coverage under Part D has undergone notable changes this year. While premiums vary by plan and are not to be discussed here, some cost factors are universal in 2025.
-
Deductible: Up to $590 annually
-
Out-of-Pocket Cap: The biggest update is the $2,000 annual cap on out-of-pocket drug costs. After reaching this limit, your plan pays 100% of covered prescription costs for the rest of the year.
While this cap brings relief, reaching it still requires significant spending. Be sure you understand how your medications fit into your plan’s formulary and tiers.
Don’t Forget About These Other Medicare Expenses
While Parts A, B, and D form the foundation, they aren’t the full story. Many people also pay for supplemental coverage and experience unexpected costs from services Medicare doesn’t fully cover.
Medicare Advantage (Part C)
While you may have heard of Medicare Advantage plans offering extra benefits, what’s often overlooked is the variability in out-of-pocket costs. Premiums vary, and enrollees must still pay the Part B premium. In-network and out-of-network charges, prior authorizations, and benefit restrictions can all influence your total cost.
Medicare Supplement (Medigap)
Medigap plans are designed to help cover costs like Part A coinsurance or Part B copayments. These plans come with their own premiums, which are not regulated like traditional Medicare. They do not include prescription drug coverage, so Part D enrollment is still necessary.
Late Enrollment Penalties
Failing to enroll in Medicare on time can cost you for life.
-
Part B Penalty: If you delay enrollment without other credible coverage, your premium increases 10% for each 12-month period you were eligible but didn’t enroll.
-
Part D Penalty: A penalty accrues if you go more than 63 days without creditable drug coverage after your Initial Enrollment Period. The penalty is calculated as 1% of the national base premium times the number of months you were uncovered.
These penalties are permanent and get more expensive the longer you delay.
How Out-of-Pocket Maximums Work in 2025
Original Medicare (Parts A and B) does not have an out-of-pocket maximum. This means your 20% coinsurance can stack up quickly with no ceiling. That’s one reason why many people opt for supplemental or Medicare Advantage coverage.
Medicare Advantage plans, by law, must include an annual maximum out-of-pocket (MOOP) limit:
-
In-network services: Up to $9,350
-
Combined in- and out-of-network services: Up to $14,000
While these plans offer some financial protection, it’s important to realize that these limits apply only to covered services and only within the plan’s rules.
Timing Matters: Enrollment Periods and Their Impact
If you want to avoid penalties and gaps in coverage, you need to understand the key Medicare enrollment timelines in 2025.
-
Initial Enrollment Period (IEP): Begins 3 months before the month you turn 65 and ends 3 months after.
-
General Enrollment Period (GEP): January 1 to March 31 each year, with coverage starting July 1. Penalties may apply if you missed IEP.
-
Annual Enrollment Period (AEP): October 15 to December 7 for making changes to Part D or Medicare Advantage.
-
Special Enrollment Periods (SEPs): Triggered by life events like losing employer coverage or moving.
Missing these windows can result in penalties, delayed coverage, or both.
Understanding the Role of Income in What You Pay
Your income plays a big role in how much you pay for Medicare, especially when it comes to Parts B and D.
In 2025, the income thresholds for IRMAA (Income-Related Monthly Adjustment Amounts) are as follows:
-
Individuals: Over $106,000
-
Couples (filing jointly): Over $212,000
If your income exceeds these levels, you’ll pay higher premiums for Part B and Part D. Medicare uses your tax return from two years prior (2023) to determine your 2025 premiums. If your income has dropped since then due to retirement or another life change, you can file a reconsideration request.
Planning Ahead Can Help You Save
Medicare planning isn’t something you do once and forget. It requires annual review and strategy. Here’s how you can manage your costs better:
-
Review your plan every year during the Annual Enrollment Period. Formularies and provider networks change.
-
Consider your medication list and see how different plans cover them.
-
Keep your income in mind, especially if you’re near an IRMAA threshold. Tax strategies could help you stay below premium brackets.
-
Think long-term: Some years you might pay more upfront to avoid unexpected bills later.
Medicare Will Cost You—But You Have Options
The truth is, Medicare in 2025 isn’t free, and it isn’t simple. It’s a structured, tiered system that can offer excellent coverage—but only if you know how to work within it. From premiums and deductibles to penalties and caps, each choice you make impacts your bottom line.
If you feel overwhelmed or unsure, speak with a licensed insurance agent listed on this website. They can help you compare plans, understand enrollment periods, and determine which options fit your health and financial goals.