Key Takeaways
-
In 2025, Medicare provides more robust mental health support than ever before, including expanded provider access and prescription drug protections.
-
You may now receive services from licensed counselors and therapists, get virtual mental health care at home, and benefit from a $2,000 annual out-of-pocket drug cost cap.
Understanding the Full Scope of Mental Health Support in 2025
Medicare has historically offered limited support for mental health care, often leaving gaps in access to therapy, psychiatric care, and medication. That changed significantly with recent reforms. In 2025, Medicare now requires broader mental health coverage, including services that used to be out of reach for many beneficiaries. Whether you are newly diagnosed or managing a long-term condition, understanding the full scope of benefits available to you is essential.
Expanded Access to Mental Health Professionals
A key improvement in 2025 is that Medicare Part B now covers services from a wider range of mental health providers. You no longer need to rely solely on psychiatrists or psychologists. Medicare now pays for services from:
-
Licensed Marriage and Family Therapists (LMFTs)
-
Licensed Mental Health Counselors (LMHCs)
-
Clinical Social Workers
-
Clinical Psychologists
-
Psychiatrists
This change increases your chances of finding a qualified provider, especially if you live in a rural or underserved area. As long as the provider accepts Medicare assignment, your sessions will be covered under Part B.
What Services Are Covered Under Medicare Part B
Medicare Part B now supports a comprehensive range of outpatient mental health services, including:
-
Individual therapy
-
Group therapy
-
Psychiatric evaluations and diagnostic testing
-
Medication management and psychotherapy combined sessions
-
Partial Hospitalization Programs (PHPs)
-
Intensive Outpatient Programs (IOPs)
-
Preventive depression and substance use screenings
To access these services, you usually need to have a mental health diagnosis and receive care from a Medicare-approved provider. Your provider must establish a plan of care and update it regularly.
Cost Sharing for Mental Health Outpatient Care
In 2025, you pay 20% of the Medicare-approved amount for outpatient mental health services after meeting the annual Part B deductible of $257. Medicare pays the remaining 80%. If you have a Medicare Supplement (Medigap) plan, it may cover some or all of your share.
Mental Health Hospitalization: What Part A Covers
If you are hospitalized for a mental health condition, Medicare Part A covers your inpatient care. This includes stays in a general hospital or a psychiatric hospital.
Key details for 2025:
-
You pay the Part A deductible of $1,676 per benefit period
-
Days 1–60: No coinsurance
-
Days 61–90: $419 daily coinsurance
-
Days 91–Lifetime reserve days (up to 60 total): $838 daily coinsurance
You can be hospitalized in a psychiatric facility for up to 190 lifetime days. After that, coverage is only available in a general hospital setting.
Telehealth for Mental Health: Expanded and Permanent
As of 2025, Medicare permanently covers mental health telehealth services provided via video or audio-only formats. You can receive therapy from the comfort of your home without traveling long distances or sitting in waiting rooms.
Medicare covers the following telehealth mental health services:
-
Initial diagnostic interviews
-
Individual or group therapy
-
Psychiatric medication management
To qualify, you must have an established relationship with the provider. Additionally, an in-person visit must occur every 12 months, beginning October 1, 2025, although certain hardship or geographic exceptions apply.
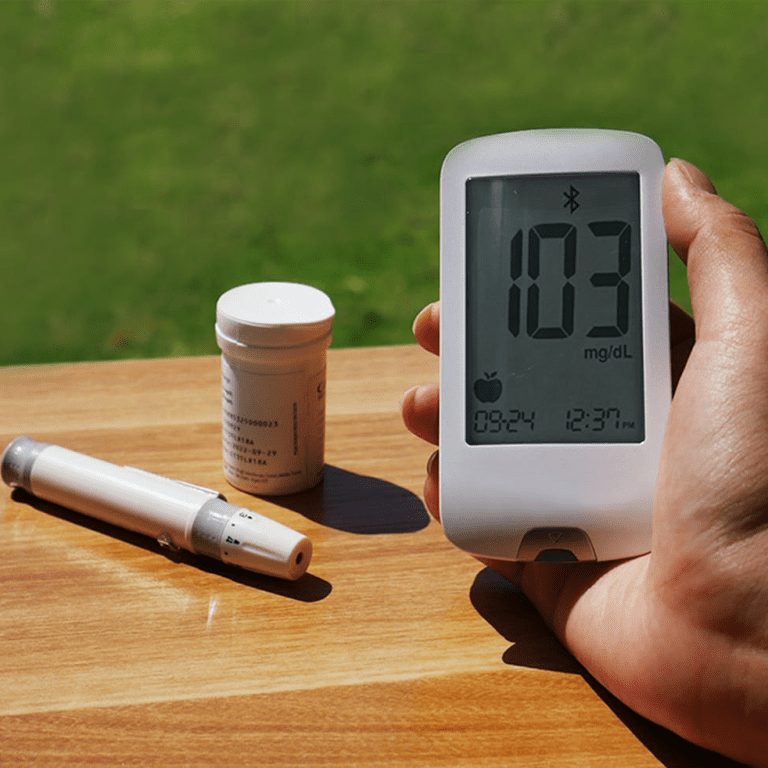
Prescription Drug Coverage for Mental Health Conditions
Medications often form the foundation of mental health treatment. In 2025, Medicare Part D and equivalent drug coverage under Medicare Advantage plans now include more protections for beneficiaries with high drug costs.
The $2,000 Out-of-Pocket Cap
You no longer face unlimited costs for brand-name or specialty psychiatric medications. Starting in 2025:
-
There is a $2,000 cap on annual out-of-pocket drug spending
-
Once you hit the cap, your plan covers 100% of covered drug costs for the rest of the year
-
The coverage gap (“donut hole”) has been eliminated
This is a significant relief if you rely on costly medications such as antidepressants, antipsychotics, mood stabilizers, or anti-anxiety drugs.
Spreading Costs Over Time
You can also opt into Medicare’s new prescription payment program. It allows you to pay for covered medications in equal monthly installments over the year, instead of paying a large amount up front at the pharmacy.
Managing Long-Term Therapy and Counseling
Medicare does not set a limit on the number of mental health therapy sessions you can have per year, as long as they are medically necessary and documented. However, your provider must follow a plan of care, and Medicare may periodically review your case to ensure ongoing need.
If your condition requires long-term counseling, here are key points to keep in mind:
-
You may see the same provider regularly if they are enrolled in Medicare
-
Group therapy is covered if it meets Medicare guidelines
-
Your provider must document progress and reevaluate your plan at least every 90 days
Preventive Screenings and Early Intervention
Preventive care now plays a larger role in mental health under Medicare. You are entitled to the following preventive mental health screenings every year:
-
Depression screening during your annual wellness visit
-
Alcohol misuse screening
-
Opioid use disorder screening
These screenings are covered at no cost to you when performed by a provider who accepts Medicare assignment. If results indicate a problem, follow-up services are covered under standard mental health benefits.
Coordinated Care Through Medicare Advantage
If you are enrolled in a Medicare Advantage plan, you still receive all the mental health benefits included in Original Medicare. In 2025, many Medicare Advantage plans also offer extra services such as:
-
Care coordination for behavioral health and primary care
-
Wellness programs focused on mental well-being
-
Nurse helplines and case management
However, these plans may have provider networks or require prior authorization, so it’s important to understand the structure of your individual plan. Check with your plan’s summary of benefits or call for clarification.
Challenges with Access to Mental Health Services
Despite these improvements, you may still face some access challenges in 2025:
-
Shortage of Medicare-approved therapists in some areas
-
Wait times to begin therapy may be long
-
Not all mental health professionals participate in Medicare
To improve your access:
-
Use the Medicare.gov provider search tool
-
Ask your primary care provider for referrals
-
Consider telehealth options, especially if you’re in a rural area
Preparing for Mental Health Coverage Reviews
Medicare periodically reviews mental health claims to ensure services are appropriate and necessary. Be prepared to:
-
Ensure your therapist documents your diagnosis and treatment plan
-
Attend regular sessions as scheduled
-
Cooperate with your provider in updating progress notes
If Medicare denies a claim, you have the right to appeal. Your provider can help by submitting additional documentation or justifying medical necessity.
How to Start Receiving Covered Mental Health Services
If you believe you need mental health support and want to use your Medicare benefits, here are the first steps:
-
Speak to your primary care doctor: They can perform screenings and provide a referral
-
Search for a Medicare-approved mental health provider: Use Medicare’s official directory
-
Call your plan (if you have Medicare Advantage or Part D): Understand how benefits apply and whether prior authorization is needed
-
Schedule your first appointment: Your provider will create a treatment plan and begin therapy
-
Follow through on the plan: Attend sessions, take prescribed medication, and communicate openly with your provider
Why Staying Informed Matters More Than Ever
Mental health care under Medicare has evolved in ways that were not available even a few years ago. These improvements offer meaningful support to help you manage anxiety, depression, substance use disorders, and other conditions. However, the system still requires you to be proactive in understanding your benefits, choosing the right provider, and following through on your care.
If you’re unsure about where to start or how your current coverage supports mental health, speak to a licensed agent listed on this website. They can guide you through the process and help ensure you are making the most of your benefits.