Part D: Prescription Drug Coverage
Introduction: Navigating Medicare Part D Prescription Drug Coverage
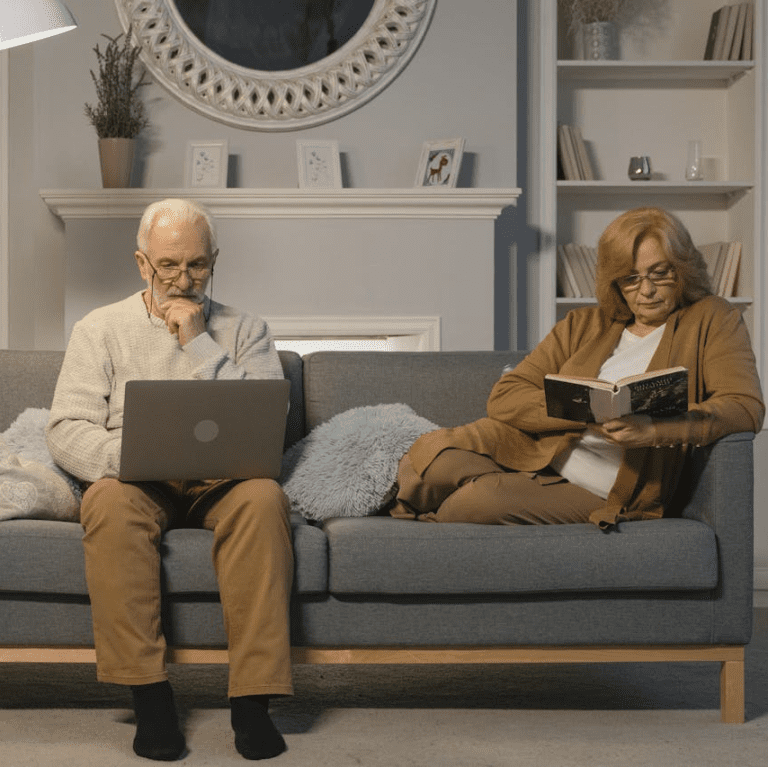
Medicare Part D offers essential prescription drug coverage for beneficiaries, ensuring access to necessary medications to manage their health conditions effectively. Understanding the nuances of Medicare Part D prescription drug coverage, including eligibility requirements, coverage options, formularies, and cost-saving strategies, is crucial for beneficiaries to make informed decisions about their medication needs. In this guide, we’ll delve into the details of Medicare Part D, empowering beneficiaries to navigate their prescription drug coverage with confidence.
Eligibility for Medicare Part D Coverage
To qualify for Medicare Part D prescription drug coverage, beneficiaries must meet certain eligibility criteria:
- Enrollment in Medicare: Beneficiaries must be enrolled in Medicare Part A and/or Part B to be eligible for Medicare Part D coverage. Most individuals become eligible for Medicare at age 65, although some may qualify earlier due to disability or certain medical conditions.
- Residency in the United States: Beneficiaries must reside in the United States, including its territories, to be eligible for Medicare Part D coverage. International travel or residence outside of the United States may impact eligibility for Part D coverage.
- Enrollment in a Stand-Alone Prescription Drug Plan (PDP) or Medicare Advantage Plan with Prescription Drug Coverage: Beneficiaries must actively enroll in a standalone Medicare Prescription Drug Plan (PDP) or a Medicare Advantage plan with prescription drug coverage (Part C) to receive Part D benefits.
Meeting these eligibility criteria ensures beneficiaries can access Medicare Part D coverage and obtain affordable prescription medications to manage their healthcare needs.
Coverage Options Under Medicare Part D
Medicare Part D offers two primary coverage options for beneficiaries:
- Stand-Alone Prescription Drug Plans (PDPs): PDPs are standalone insurance plans that provide coverage for prescription medications. Beneficiaries enrolled in Original Medicare (Parts A and B) can enroll in a PDP to obtain prescription drug coverage while retaining their Original Medicare benefits.
- Medicare Advantage Prescription Drug Plans (MA-PDs): MA-PDs are Medicare Advantage plans that include prescription drug coverage as part of their comprehensive benefits package. Beneficiaries enrolled in Medicare Advantage (Part C) can choose a MA-PD to receive both medical and prescription drug coverage through a single plan.
Understanding the coverage options under Medicare Part D allows beneficiaries to choose the plan that best fits their medication needs and healthcare preferences.
Medicare Part D Formularies
Medicare Part D plans maintain formularies, which are lists of covered prescription drugs and their associated costs. Here are some key aspects of Medicare Part D formularies:
- Formulary Tiers: Formularies categorize drugs into different tiers based on their cost and coverage level. Tier 1 typically includes generic drugs with the lowest copayments, while higher tiers may include brand-name drugs or specialty medications with higher copayments or coinsurance.
- Drug Coverage Determination: Part D plans determine which drugs are covered and at what cost based on factors such as clinical effectiveness, safety, and cost-effectiveness. Beneficiaries should review their plan’s formulary to ensure their prescribed medications are covered and affordable.
- Prior Authorization and Step Therapy: Some medications may require prior authorization or step therapy before they are covered by Part D plans. Prior authorization requires approval from the plan for certain medications, while step therapy may require beneficiaries to try lower-cost alternatives before accessing certain drugs.
Understanding the formulary and coverage determination process under Medicare Part D helps beneficiaries navigate their medication needs and optimize their drug coverage.
Cost-Saving Strategies for Medicare Part D
To minimize out-of-pocket costs and maximize savings on prescription medications under Medicare Part D, beneficiaries can consider the following strategies:
- Generic Substitutions: Whenever possible, opt for generic medications instead of brand-name drugs to save on copayments or coinsurance. Generic drugs are equivalent in quality and effectiveness to brand-name drugs but are typically available at a lower cost.
- Preferred Pharmacies: Some Part D plans offer preferred pharmacy networks where beneficiaries can access discounted copayments or coinsurance for prescription medications. Use preferred pharmacies within your plan’s network to maximize savings on medications.
- Medication Therapy Management (MTM) Programs: Many Part D plans offer MTM programs to help beneficiaries manage their medications more effectively, optimize drug therapy, and prevent adverse drug interactions. Take advantage of MTM services to receive personalized support and guidance from pharmacists.
- Extra Help Program: Low-income beneficiaries may qualify for the Extra Help Program, also known as the Low-Income Subsidy (LIS) program, which provides financial assistance with prescription drug costs, including premiums, deductibles, copayments, and coinsurance.
By implementing these cost-saving strategies, beneficiaries can reduce their out-of-pocket expenses and access necessary medications affordably under Medicare Part D.
Coverage Gap (Donut Hole) in Medicare Part D
Beneficiaries should be aware of the coverage gap, also known as the “donut hole,” in Medicare Part D prescription drug coverage. The coverage gap is a temporary period during which beneficiaries may pay higher out-of-pocket costs for prescription medications before catastrophic coverage begins. Here’s how the coverage gap works:
- Initial Coverage Period: Beneficiaries pay a deductible (if applicable) and copayments or coinsurance for covered medications until their total drug costs reach the initial coverage limit set by their Part D plan.
- Coverage Gap: Once beneficiaries reach the initial coverage limit, they enter the coverage gap, where they are responsible for a higher percentage of their drug costs. During the coverage gap, beneficiaries pay a discounted percentage (e.g., 25%) of the cost of brand-name drugs and a lower percentage (e.g., 25%) of the cost of generic drugs until they reach the out-of-pocket threshold.
- Catastrophic Coverage: Once beneficiaries reach the out-of-pocket threshold, they qualify for catastrophic coverage, where they pay a reduced coinsurance or copayment amount for the remainder of the calendar year.
Understanding the coverage gap and its implications for prescription drug costs can help beneficiaries plan and budget accordingly for their medication expenses under Medicare Part D.
Conclusion: Maximizing Medication Coverage with Medicare Part D
Medicare Part D prescription drug coverage plays a vital role in helping beneficiaries access necessary medications to manage their health conditions effectively. By understanding eligibility requirements, coverage options, formularies, cost-saving strategies, and the coverage gap, beneficiaries can navigate their medication needs with confidence and ensure affordable access to prescription drugs under Medicare Part D.
Empower yourself with knowledge, review your Medicare Part D options, and choose a plan that meets your medication needs and budget. Remember, licensed insurance agents and valuable resources are available to provide personalized assistance and support throughout your Medicare journey. Ready to explore your Medicare Part D prescription drug coverage options? Download our free eBook.
Contact Information:
Email: [email protected]
Phone: 7025556789