Key Takeaways
-
Medicare Advantage plans often offer extra benefits, but you must carefully examine the fine print to understand what is actually covered and what limitations may apply.
-
In 2025, certain changes in Medicare regulations and out-of-pocket cost caps make it even more important to review every detail of a plan before enrolling.
The Surface Appeal of Medicare Advantage Plans
Medicare Advantage, also known as Medicare Part C, continues to attract millions of enrollees in 2025. The reason is clear: these plans often advertise extra benefits like dental, vision, and hearing coverage in addition to what Original Medicare provides. They may also offer prescription drug coverage and perks like wellness programs or gym memberships.
But appealing as they sound, these benefits come with conditions. Each plan is operated by a private company approved by Medicare, and the actual coverage can vary significantly depending on where you live, the provider’s network rules, and how the plan is structured.
What Medicare Advantage Must Cover
Every Medicare Advantage plan must include the core services covered by Original Medicare:
-
Inpatient hospital care (Part A)
-
Outpatient medical care (Part B)
These include:
-
Doctor visits
-
Lab tests
-
Surgeries
-
Hospital stays
-
Preventive screenings
Plans may also include Medicare Part D prescription drug coverage and supplemental benefits, but those are not standardized and require closer attention.
The Importance of Plan Networks in 2025
In 2025, most Medicare Advantage plans still operate as HMOs or PPOs. That means they rely on a specific network of doctors, hospitals, and other health providers. If you go outside the network, your care might not be covered—or it might come at a significantly higher cost.
Before enrolling, ask yourself:
-
Are your current doctors in the plan’s network?
-
Will you need referrals to see specialists?
-
How far are the nearest in-network hospitals or urgent care centers?
If you split time between two states or travel often, a plan with a narrow network could leave you without coverage when you need it most.
Why Out-of-Pocket Costs Still Matter
It’s easy to get drawn to Medicare Advantage plans that advertise low monthly premiums. But premiums are just one piece of the cost puzzle. You also need to consider deductibles, copayments, and coinsurance.
In 2025, Medicare Advantage plans have a maximum out-of-pocket (MOOP) limit of $9,350 for in-network services and $14,000 for combined in- and out-of-network services. But not all plans offer out-of-network benefits, and some may come close to hitting these limits if you require ongoing care.
Look closely at the:
-
Annual deductible (if applicable)
-
Copayments for primary and specialty care
-
Emergency room or hospital admission fees
-
Coinsurance for services like physical therapy or outpatient surgery
These costs can add up quickly, especially for chronic or complex health needs.
How Prior Authorization Can Delay Your Care
One of the most commonly overlooked features of Medicare Advantage plans is prior authorization. In 2025, many plans still require prior approval for certain services such as MRIs, surgeries, or home health care. This process can delay access to care or result in denial if the plan doesn’t deem the service medically necessary.
If you’re managing multiple conditions or need frequent specialist care, prior authorization can create unnecessary hurdles. Before enrolling, it’s important to check:
-
Which services need prior authorization
-
How long the approval process typically takes
-
Whether previous patients have experienced delays or denials
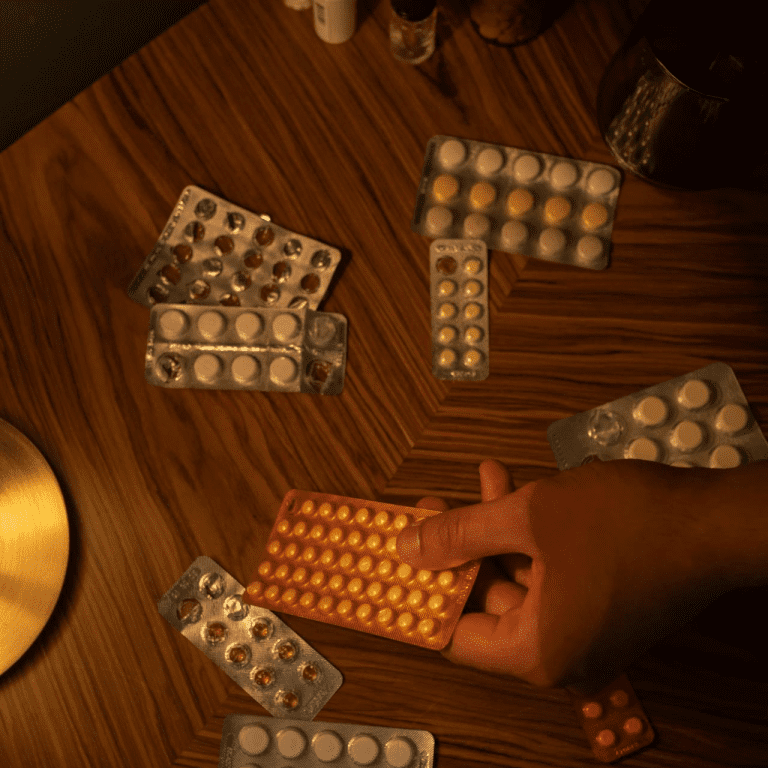
The Drug Coverage Fine Print
Many Medicare Advantage plans include Part D drug coverage, but not all formularies (drug lists) are the same. The drugs covered, the tiers they fall into, and the copayment structure can vary widely. In 2025, you must also consider how a plan handles the new $2,000 out-of-pocket cap for prescription drugs.
Key points to review:
-
Does the plan cover your current medications?
-
Are your drugs placed on a high-cost tier?
-
Is prior authorization required for your prescriptions?
-
Are there preferred pharmacies that offer lower costs?
Choosing a plan without verifying drug coverage can leave you paying much more out of pocket than you expected.
Supplemental Benefits: Nice but Not Guaranteed
Medicare Advantage plans often advertise extras like:
-
Routine dental cleanings
-
Vision exams and eyeglasses
-
Hearing aids
-
Fitness memberships
-
Transportation to medical appointments
In 2025, these benefits are still not standardized across plans. Some plans offer them in full, others in part, and some only under specific conditions. For instance, your dental benefit may cover cleanings but not root canals. Or your hearing aid allowance may apply only to certain brands or providers.
Before relying on these extras, review:
-
Coverage limits (dollar amount or service frequency)
-
Approved providers
-
Waiting periods or exclusions
Just because a plan mentions a benefit doesn’t mean you’ll receive full or affordable access to it.
Plan Changes Happen Every Year
Medicare Advantage plans are allowed to make changes each year, including to:
-
Premiums
-
Deductibles
-
Drug formularies
-
Provider networks
-
Supplemental benefits
In 2025, all these variables are still at play. That’s why it’s crucial to read your Annual Notice of Change (ANOC) each fall and compare your plan with others during the Medicare Open Enrollment Period from October 15 to December 7.
If you stay in a plan without reviewing the new terms, you could be caught off guard by increased costs or reduced coverage starting January 1 of the following year.
Enrollment Rules You Need to Know
Once you enroll in a Medicare Advantage plan, your flexibility to change plans is limited. In most cases, you’re locked in for the calendar year unless you qualify for a Special Enrollment Period. You do get another chance during the Medicare Advantage Open Enrollment Period (January 1 to March 31), but you can only make one switch during that time.
This means any surprises after enrollment—like a drug not being covered or a doctor leaving the network—may leave you stuck until the next year.
Is a Medicare Advantage Plan Right for You?
There’s no one-size-fits-all answer. Medicare Advantage may work well if:
-
Your preferred doctors and hospitals are in the network
-
You’re relatively healthy and want to take advantage of extra benefits
-
You understand and can budget for the out-of-pocket limits
But it might not be the best fit if:
-
You travel often or spend time in multiple states
-
You have chronic conditions requiring frequent specialist care
-
You prefer not to deal with referrals and prior authorizations
Why Careful Reading Matters in 2025
Medicare Advantage plans in 2025 are full of fine print—sometimes in footnotes, sometimes in pages of plan documents. You’ll only uncover the real costs, restrictions, and processes if you read them closely.
Here’s what to read before enrolling:
-
The Summary of Benefits
-
The Evidence of Coverage (EOC)
-
The Provider Directory
-
The Drug Formulary
Use these resources to compare plans, clarify confusing terms, and ask questions.
Make Your Decision Based on Facts, Not Promises
At a glance, Medicare Advantage plans may look alike. But once you dig into the details, you’ll see meaningful differences in costs, coverage, flexibility, and access to care. That’s why your decision should be based on the facts—not the headlines or promotional materials.
If you need help interpreting those facts, you’re not alone. Speak to a licensed agent listed on this website to get personalized advice before you enroll.